Palliate
Safely support timely end-of-life symptom management in the home
Medication administration, training and education designed to keep patients safely at home at the end of life
“I couldn’t have kept her at home without this. She wouldn’t have been able to die at home without it.”
– Carer, London

the problem
64% of people with cancer would like to die at home, but they face a range of problems
Source: The Final Injustice: Variation in end of life care in England, Macmillan (2017)
patients wait too long for relief
Most community teams cannot offer true 24/7 coverage so people have to wait longer than they should to have their symptoms managed at home.
families faced with unmanaged symptoms can panic
Carers and patients can become distressed and families lose control of the situation, resulting in unplanned hospital admission which can often lead to death away from home.
health providers lack policies and practices to help
There is a lack of widespread, well-evidenced and easily accessible policies and practices around carer-led symptom management.
the solution
An intervention that empowers lay carers to provide end-of-life symptom relief, with professional support
higher confidence
Provides carers with the skills and confidence they need to administer subcutaneous injections, enabling them to better manage symptoms until their loved one dies.
effective, efficient support
Enables teams to provide remote support to reduce friction and delays in the experience of administering medications, reducing travel time, team resources and overall cost.
improved safety for everyone
A single evidence-based digital-and-physical solution that can be deployed within NHS Trusts and other health settings, providing robust data collection for quality improvement and improved patient safety.
Findings from our pre-pilot with CNWL NHS Trust
24 minutes
Average time between symptom onset and administration of medication
8.8 out of 10
Average confidence
score of lay carers administering medications
80%
Percentage of medications given by lay carers without any healthcare professional help being sought
Palliate is designed around carer and professional needs
We are an interdisciplinary group of designers, technologists, clinicians and researchers. We use human-centred design to rapidly dissect problems, identify opportunities, and develop clinically-evaluated digital solutions. We work with carers with lived experience to inform our work, and centre our development around their needs. We are an integral part of the Institute of Global Health Innovation at Imperial College London.

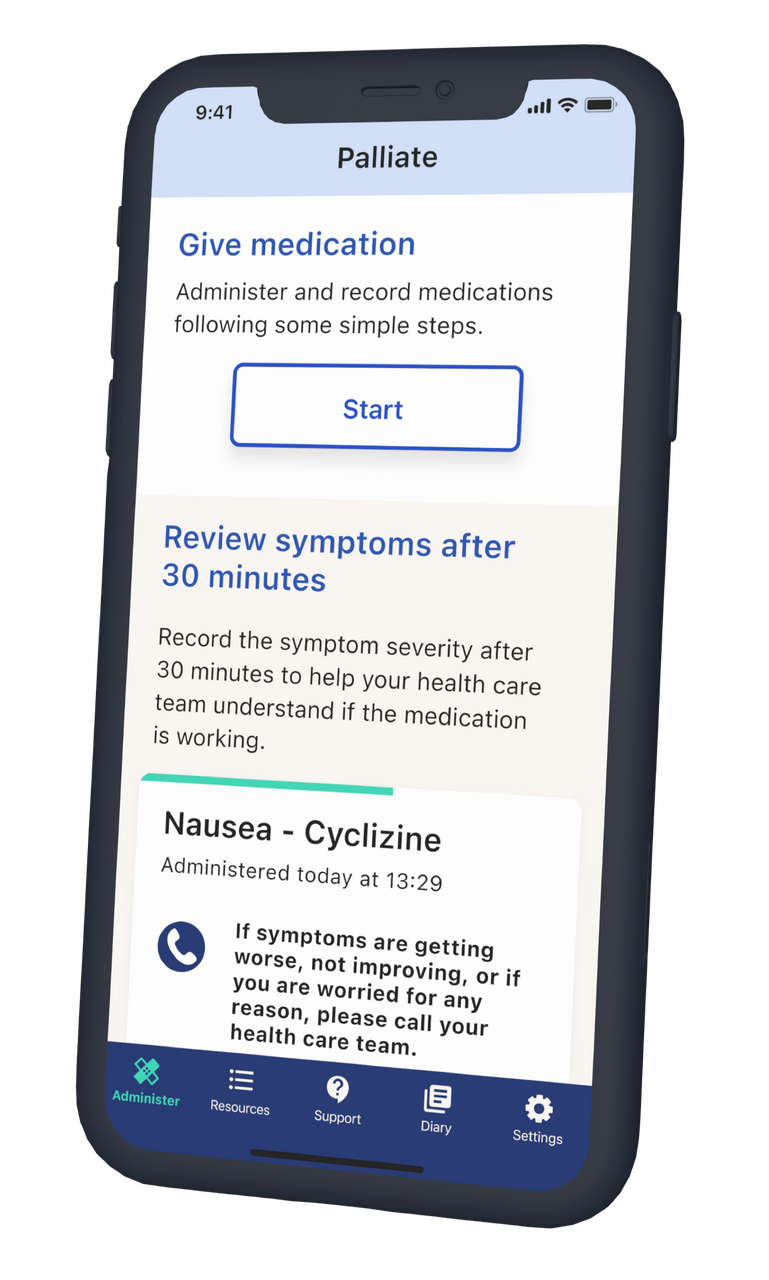
using palliate
If you are a clinician working in an NHS Trust or hospice across the UK, you are invited to join our waiting list to register interest in using Palliate where you work.Please note, that although Palliate is designed to be used by lay carers, our waiting list is for healthcare professionals only and Palliate cannot be used without clinical supervision and training.
community of practice
Real lasting change takes more than technology. The UK is a diverse country, with different healthcare systems and communities. It will take everyone to support a change like this.We have a community of practice to ensure that everyone’s voice is heard, and that Palliate responds to the needs of families and healthcare teams across the UK.
Developed in partnership and collaboration with



2022 © Imperial College London. All rights reserved.
No part of this site may be reproduced in whole or in part in any manner without the permission of the copyright owner.
palliate
Hear what carers say
“I was able to improve symptoms, pain, distress, nausea… the ability to give an injection made a massive difference. There was no way to stop the whole thing - them dying at home - from being stressful, but it was helpful to be in control. In some ways I felt calmer knowing and being in charge.”– Carer, London
Radio 4's Inside Health recently explored how friends and family are being trained to administer medications, to ease loved ones' symptoms at the end of life.
palliate
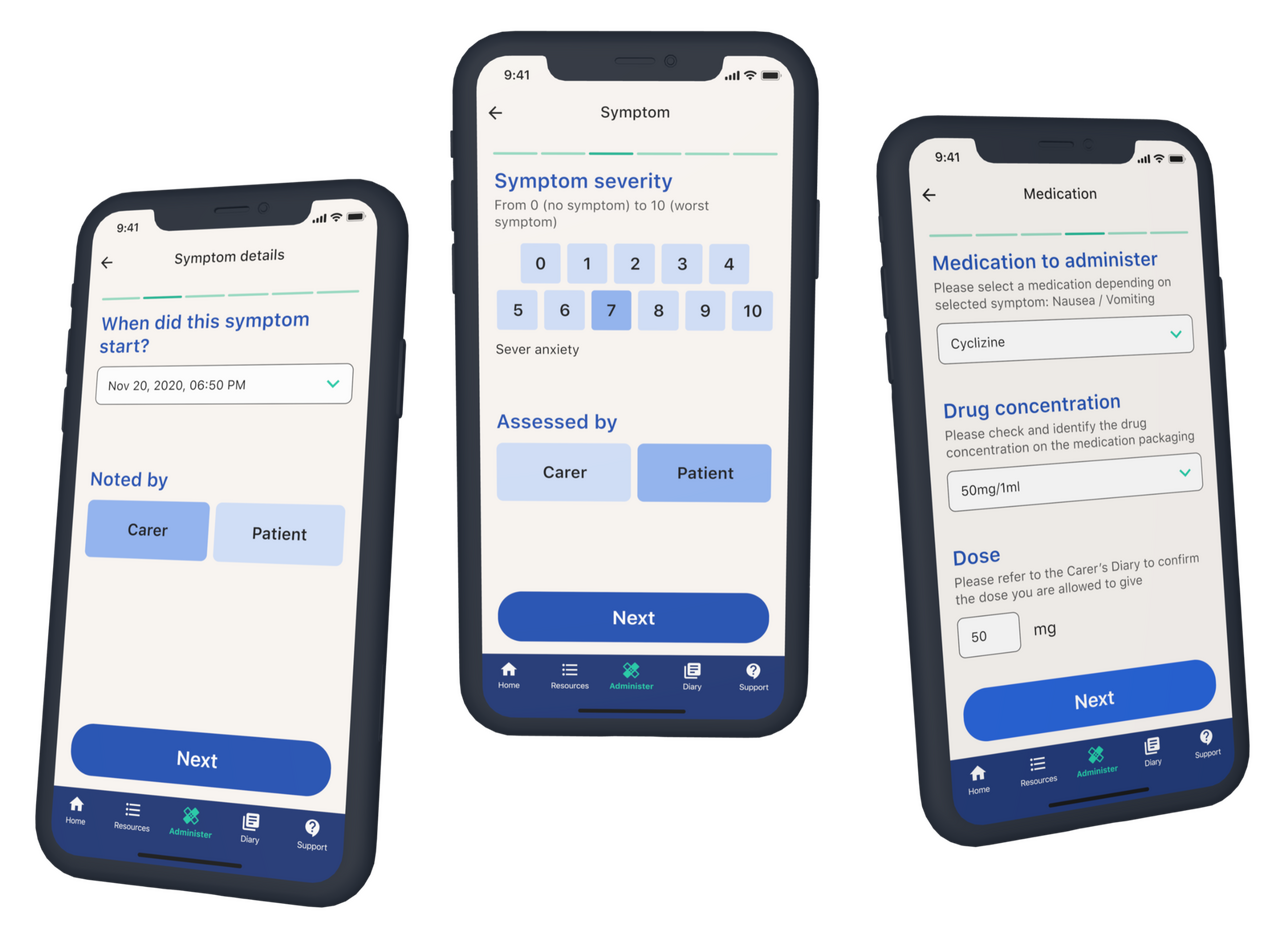
How it works
identification
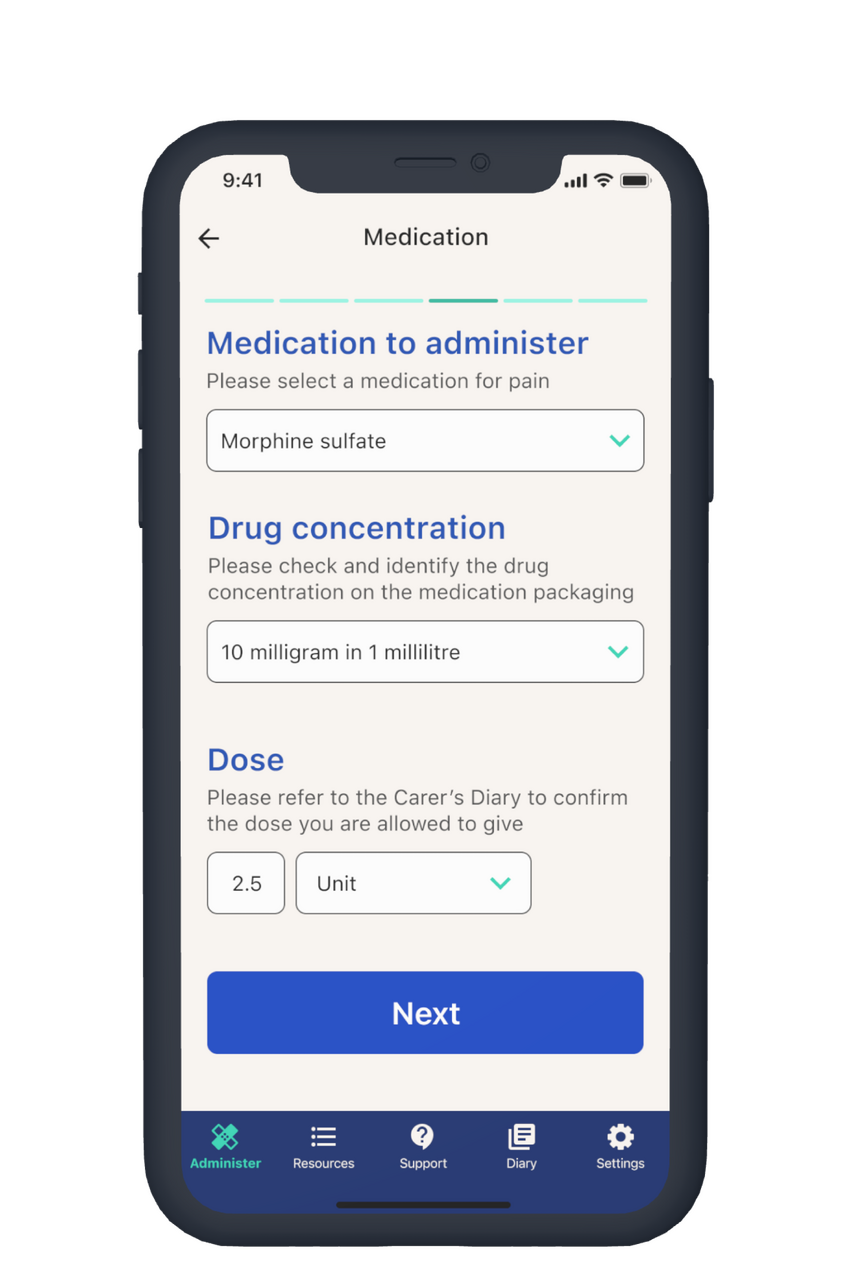
Carers can record symptoms (including onset and severity) and record prescribed medications (dose, concentration) for each symptom.
administration
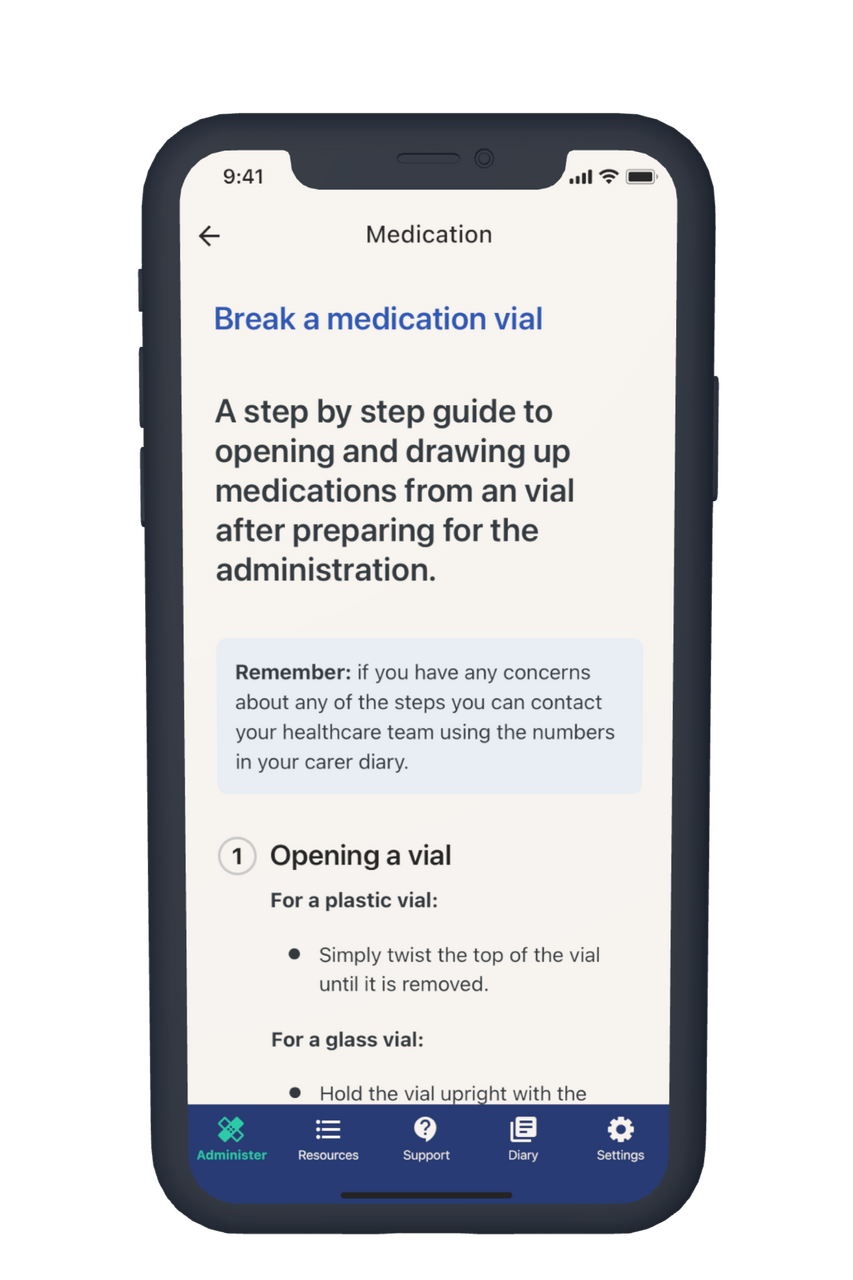
Each step of preparation and administration is broken down into easy-to-use guides that carers can use to confidently administer sub-cutaneous injections.
education
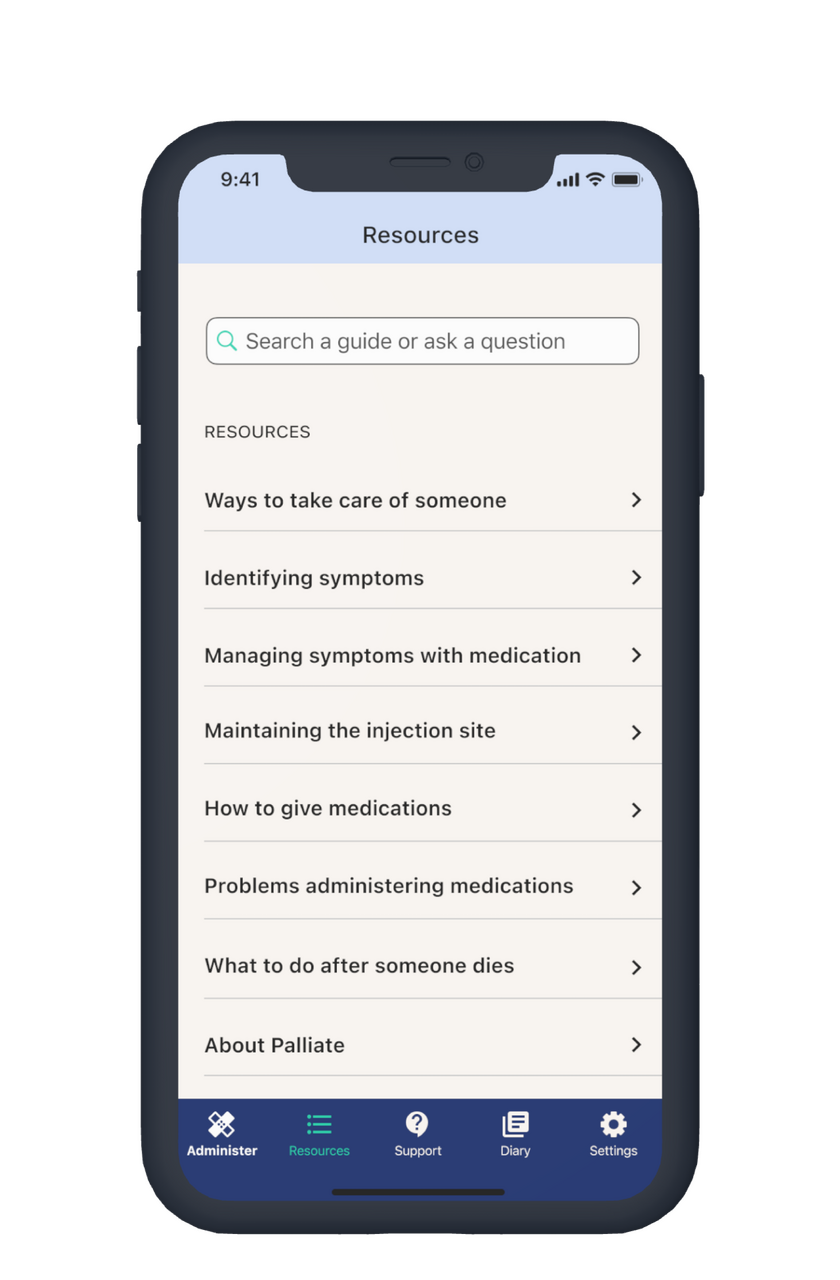
A rich resource of knowledge and skills to care for a dying person are within easy reach and remote support with professional is provided via phone lines.